Introduction:
One of the most urgent public health emergencies of our day is the opioid epidemic, which is defined by a sharp surge in opioid usage, addiction, and overdose deaths. The extensive prescribing of opioid painkillers, which was initially motivated by the medical community’s desire to better treat pain, has had major unexpected consequences. It’s still very difficult to strike a balance between the risk of addiction and the requirement for efficient pain management. This article examines the intricacies of the opioid crisis, the signs and dangers of opioid usage, and possible methods for controlling pain while reducing the risk of addiction.
The Narcotic Epidemic’s Ascent:
Pharmaceutical firms told the medical community that patients would not become hooked to prescription opioid painkillers, which set the stage for the opioid epidemic in the late 1990s. As a result, more opioid prescriptions were written to treat pain. But as time went on, it became clear that opioids have a high risk of addiction, and abuse of these drugs increased dramatically. The pandemic has progressed through three waves: prescription opioids drove the first wave, heroin drove the second, and synthetic opioids like fentanyl, which are far more potent and lethal, drove the third wave.
Effective pain management and the danger of addiction must be balanced, and this necessitates a complex strategy. When possible, healthcare professionals should think about non-opioid alternatives while closely evaluating the patient’s pain. When prescribing opioids, the lowest effective dose for the shortest amount of time is best. It is vital to inform patients about the dangers and responsible usage of opioids. A balanced approach to pain management also includes supporting individuals who develop addicted and keeping an eye out for indications of overuse on the part of the patient.
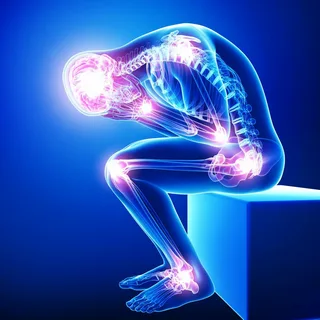
Symptoms and hazards of Opioid Use:
Although opioids are a useful treatment for both acute and chronic pain, using them has a number of serious hazards. exhilaration, drowsiness, sedation, and pain alleviation are common signs of opioid usage. But there’s also a chance that these medications will have adverse effects like constipation, nausea, respiratory depression, and cognitive decline. Long-term use can result in physical dependency, where stopping the drug suddenly causes withdrawal symptoms, and tolerance, which requires increasing dosages to have the same effect. Addiction is a serious risk connected with opioid use, defined by obsessive drug seeking and usage despite negative effects.
The Function of Medical Professionals:
Medical professionals are essential in combating the opioid crisis. They need to be knowledgeable and proficient in both diagnosing and treating opioid use disorders as well as appropriately prescribing opioids. It is crucial to be up to date on pain treatment, addiction, and the most recent recommendations for prescription opioids. In shared decision-making, healthcare providers and patients should go over the advantages and disadvantages of opioid therapy as well as look into non-opioid pain relief choices. Prescription drug monitoring programs (PDMPs) should also be used to track opioid prescriptions and stop misuse.
Addiction Treatment and rehabilitation:
Access to efficient treatment and rehabilitation programs is crucial for people battling opioid addiction. The gold standard for treating opioid use disorder is medication-assisted treatment (MAT), which mixes behavioral and counseling therapies with drugs like methadone, buprenorphine, or naltrexone. Withdrawal symptoms, cravings, and the chance of relapsing can all be lessened with MAT. Along with addressing co-occurring mental health issues, comprehensive treatment approaches should support the restoration of relationships and functionality and encourage long-term recovery through follow-up counseling and support groups.
Non-Opioid Pain treatment Techniques:
For both acute and chronic pain, a range of non-opioid pain treatment techniques might be helpful. For a variety of ailments, acetaminophen, nonsteroidal anti-inflammatory medications (NSAIDs), and certain antidepressants and anticonvulsants can all relieve pain. Both the psychological and physical components of chronic pain can be addressed with physical therapy, exercise, and cognitive-behavioral therapy (CBT). Other alternatives for pain management without the hazards of opioids include complementary therapies including mindfulness-based stress reduction (MBSR), chiropractic adjustments, and acupuncture.
Policy and Community Interventions:
Coordinated initiatives at the community and policy levels are necessary to combat the opioid epidemic. Policies that control the prescription of opioids, facilitate access to addiction treatment, and boost the supply of naloxone—a drug that may reverse an opioid overdose—are essential. Additionally crucial are community-based therapies like public awareness campaigns, funding for harm reduction projects (such needle exchange programs), and campaigns to lessen the stigma attached to addiction. A comprehensive strategy to tackle the opioid epidemic can be developed through cooperation between law enforcement, community organizations, legislators, and healthcare providers.
Summary:
In conclusion, the opioid crisis poses a difficult problem that calls for a careful balancing act between reducing the danger of addiction and effectively relieving pain. In order to address this public health catastrophe, it is imperative that people comprehend the causes and consequences of the epidemic, identify the symptoms and hazards associated with opioid use, and adopt a multimodal approach to pain management. We can reduce opioid misuse and its devastating effects while ensuring that patients receive the compassionate and efficient pain care they require by adopting non-opioid pain management strategies, providing effective addiction treatment and recovery options, educating healthcare providers, and enacting supportive policies and community interventions.