Pain management is a complex field that addresses the needs of millions of patients dealing with chronic or acute discomfort. However, as demand grows for these services, so does the complexity of the billing and coding process. The combination of regulatory changes, payer-specific rules, and evolving coding systems presents significant hurdles for providers. Accurate billing and coding not only ensure compliance but also play a vital role in maintaining the financial health of a pain management practice.
In this blog, we’ll explore how healthcare providers can improve their pain management billing and coding processes, and we’ll dive into the key challenges they must overcome to ensure revenue cycle success.
📌 Why Pain Management Billing and Coding Matter
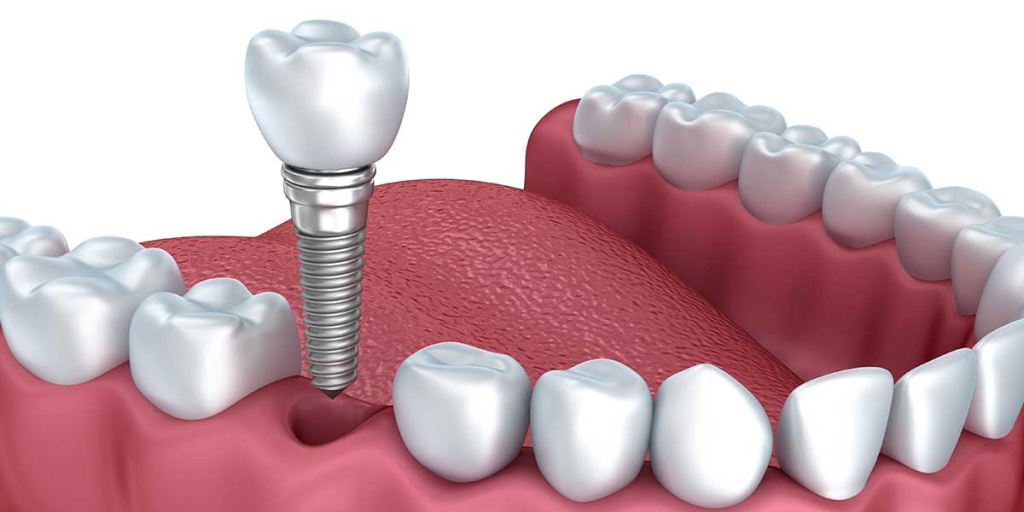
Unlike general medical billing, pain management involves intricate procedures such as epidural injections, spinal cord stimulators, nerve blocks, and multi-drug regimens. Each of these requires precise documentation and coding. Inaccurate billing can lead to denied claims, delayed payments, compliance audits, and lost revenue.
Efficient billing and coding also:
-
Ensure proper reimbursement for high-cost procedures
-
Reduce claim rejections and denials
-
Shorten the payment cycle
-
Improve patient satisfaction through transparent financial communication
✅ Strategies to Improve Pain Management Billing and Coding
1. Stay Updated on CPT and ICD-10 Code Changes
One of the biggest contributors to billing errors is the use of outdated codes. Each year, the American Medical Association (AMA) updates the CPT code set, and ICD-10 codes are often revised to reflect new diagnoses and treatments.
What to do:
-
Schedule regular coding workshops or webinars for your team.
-
Subscribe to coding newsletters from AAPC, CMS, or AMA.
-
Work with a certified medical coder who specializes in pain management.
2. Understand and Apply Modifier Rules Correctly
Pain management often involves procedures that require modifiers to explain specific circumstances—such as repeat procedures or services performed on different body parts.
Incorrect use of modifiers like -25, -59, or -RT/-LT can lead to denials or downcoding.
Tip: Create a quick-reference sheet for common modifiers used in your procedures and ensure all billing staff understand them.
3. Ensure Comprehensive and Accurate Documentation
Every claim begins with proper clinical documentation. Insufficient or vague notes can result in claim denials, delayed payments, or legal issues.
Key areas to document:
-
Medical necessity of the procedure
-
Detailed procedure notes
-
Pre- and post-procedure assessments
-
Patient response to treatment
Pro tip: Implement EMR templates tailored for pain management services to streamline consistent documentation.
4. Conduct Internal Audits Regularly
Audits help identify patterns in denied claims, underpayments, or incorrect coding practices before they become major issues. They also prepare your practice for potential payer audits.
Audit focus areas:
-
Coding accuracy
-
Modifier usage
-
Documentation completeness
-
Frequency of certain billed services
5. Use RCM Software with Built-in Compliance Rules
A robust Revenue Cycle Management (RCM) system that includes coding validation and claim scrubbers can catch common errors before claims are submitted. Features like real-time eligibility verification and pre-appointment cost estimators improve front-end processes and reduce denials.
Look for software that offers:
-
Automated eligibility checks
-
Real-time claims tracking
-
Coding suggestions
-
Alerts for missing documentation or authorization
6. Train Staff on Payer-Specific Guidelines
Every insurance provider—whether it’s Medicare, Medicaid, or private payers—has unique billing requirements for pain management services. Knowing each payer’s prior authorization process, reimbursement limits, and documentation needs is essential.
Build a payer matrix to keep track of:
-
Prior authorization rules
-
Procedure frequency limits
-
Covered vs. non-covered services
-
Appeal processes for denials
🚧 Key Challenges in Pain Management Billing and Coding
While following best practices can certainly improve your RCM performance, pain management billing presents several unique challenges that must be addressed:
🔒 1. Prior Authorization Delays
Many insurers require prior authorization before approving procedures or pain medications. Delays or denials due to missing information or lack of medical necessity can significantly disrupt revenue flow.
Solution: Assign a dedicated staff member or use software to track and manage authorizations effectively.
⛔ 2. Restrictions on Procedure Frequency
Certain injections or therapies may only be allowed a set number of times within a time frame. Billing for procedures beyond those limits—even if medically necessary—can trigger denials.
Best practice: Monitor procedure frequency per patient and payer to avoid crossing thresholds.
🕒 3. Prepayment Coding Reviews
Insurance companies may delay payments for 90 to 180 days if a claim is flagged for coding review. These delays tie up your revenue and impact cash flow.
Strategy: Submit clear and thorough documentation along with claims to reduce chances of being flagged.
💊 4. Increased Scrutiny on Pain Medications
Due to the opioid crisis, prescriptions for certain pain medications are heavily monitored. Providers must show evidence of medical necessity and prove alternative treatments were considered.
Tip: Ensure accurate drug codes and maintain proper documentation of treatment plans and medication responses.
❌ 5. No Coverage for Some Alternative Therapies
Though the CDC recommends non-pharmacologic pain therapies like acupuncture and physical therapy, many payers don’t reimburse for them, creating a gap between clinical care and compensation.
Solution: Verify insurance benefits beforehand and inform patients of any out-of-pocket responsibilities.
🏥 6. Insurance System Overload
The volume of pain-related claims and evolving rules overwhelm many insurance companies. Some delegate approvals to third-party reviewers, causing even more delays.
What you can do: Be persistent with follow-ups and maintain detailed documentation to appeal unjust denials.
💡 Additional Tips to Maximize Revenue
✔ Cater to a Diverse Patient Base
Don’t rely solely on Medicare or Medicaid. Accepting commercial and workers’ comp insurance widens your income opportunities and makes your practice more resilient.
✔ Know the Cost of Procedures
Understand the true cost of services, especially when performed in ambulatory surgical centers (ASCs) versus in-office. Compare it with expected reimbursements to make informed decisions.
✔ Engage Patients in Financial Conversations
Use cost estimators to help patients understand their financial responsibility. Offer payment plans or partial payment options upfront to reduce outstanding balances.
🔚 Final Thoughts
Pain management billing and coding require more than just knowledge—they demand precision, proactive planning, and consistent adaptation to ever-changing regulations. By implementing best practices and addressing known challenges head-on, you can streamline your revenue cycle and secure timely reimbursements.
Whether you handle billing in-house or outsource to a professional RCM provider, the key lies in education, technology, and attention to detail. Improving these processes will not only increase your revenue but also allow you to focus more on what matters most—providing excellent care to your patients.