Introduction
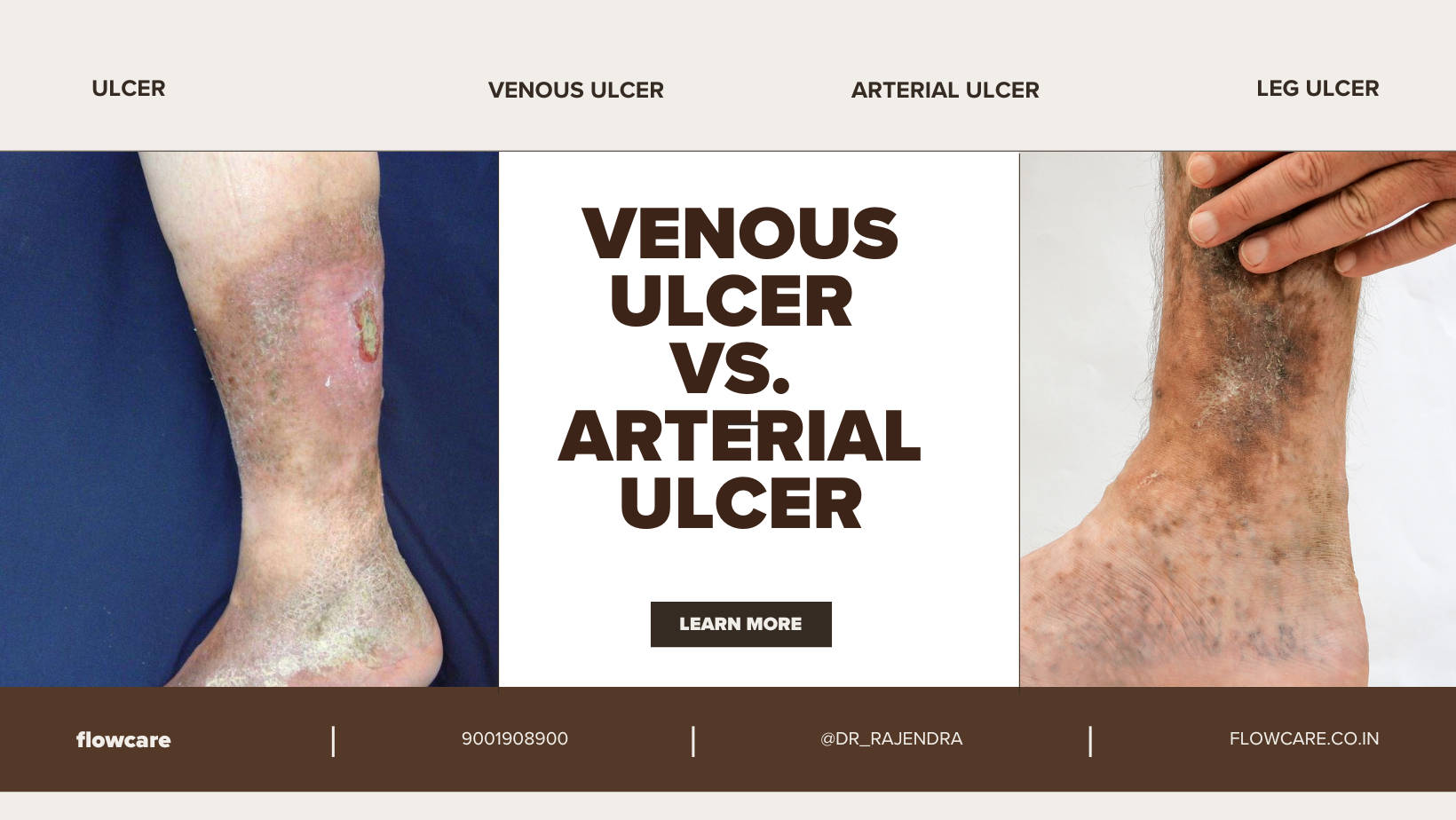
Ulcers are open sores that can develop on the skin due to poor blood flow or injury, and they come in various types. Among the most common are venous leg ulcers and arterial ulcers. Though they may appear similar on the surface, the causes, symptoms, and treatments differ significantly. Understanding these differences is crucial for effective treatment and management. In this article, we will dive deep into the topic of arterial ulcer, comparing them with venous leg ulcers and offering insights into how each can be treated.
What is an Arterial Ulcer?
An arterial ulcer is a type of wound that forms when there is insufficient blood flow to the affected area, usually due to narrowed or blocked arteries. This lack of circulation results in oxygen and nutrient deprivation, causing the skin and tissues to break down, which ultimately leads to the formation of an ulcer. Arterial ulcers are typically found on the lower legs or feet, especially on the toes, heels, or outer ankle.
These ulcers are often associated with conditions like peripheral artery disease (PAD), atherosclerosis, or diabetes, all of which impact blood flow. Because of the lack of oxygen and nutrients to the tissue, arterial ulcers can be difficult to heal and may lead to severe complications if not treated promptly.
Key Differences Between Arterial and Venous Leg Ulcers
While both arterial and venous ulcers affect the lower legs, they have distinct differences in terms of their origin, symptoms, and appearance.
1. Causes
- Arterial Ulcers: Caused by poor blood flow due to narrowed or blocked arteries, often linked to conditions like peripheral artery disease, atherosclerosis, or diabetes.
- Venous Ulcers: Develop when the veins in the legs fail to efficiently return blood back to the heart, leading to high pressure in the veins. Conditions such as chronic venous insufficiency (CVI) often cause venous ulcers.
2. Appearance
- Arterial Ulcers: These ulcers are usually smaller but deeper, with a well-defined edge. They often have a pale or yellowish base and can be covered with necrotic tissue. The surrounding skin may appear thin and shiny.
- Venous Ulcers: Typically larger, shallower, and have a more irregular shape. The base of the ulcer is usually red or yellow, and the surrounding skin might be discolored or swollen.
3. Location
- Arterial Ulcers: Most often found on the toes, heels, and outer ankles. These areas are more vulnerable due to reduced blood supply.
- Venous Ulcers: Usually occur around the lower leg, particularly near the ankle area, and may involve the calf or inner part of the leg.
4. Symptoms
- Arterial Ulcers: Often cause significant pain, especially when the legs are elevated, due to the lack of blood flow. The affected areas may feel cold to the touch, and there may be visible signs of reduced circulation, such as pale or bluish skin.
- Venous Ulcers: While they may also cause pain, venous ulcers tend to feel more like a heavy or aching sensation in the affected area. There is often swelling and a sense of tiredness in the leg.
Symptoms of Arterial Ulcers
Arterial ulcers often present with specific signs and symptoms that distinguish them from venous ulcers. Some of these include:
- Severe pain: Pain tends to be more intense, especially when the legs are elevated.
- Cold feet or legs: The affected area might feel cold to the touch due to poor circulation.
- Pale skin: The skin surrounding the ulcer may appear pale or bluish, indicating a lack of oxygenated blood.
- Shiny, thin skin: The skin around the ulcer may become thin, shiny, and hairless due to reduced blood flow.
- Delayed healing: Arterial ulcers are notoriously slow to heal, and without proper treatment, they may worsen.
Diagnosis of Arterial Ulcers
Proper diagnosis of an arterial ulcer is crucial to ensure effective treatment. Doctors typically begin with a physical examination and take a thorough medical history to check for conditions like peripheral artery disease. Some common diagnostic tests include:
- Ankle-brachial index (ABI): This test measures the blood pressure in the ankles and compares it to the blood pressure in the arms to check for signs of poor circulation.
- Doppler ultrasound: This imaging test can assess the blood flow in the arteries and help identify any blockages or narrowing.
- Angiography: In some cases, a more advanced procedure may be needed to view the blood vessels more clearly.
Treatment for Arterial Ulcers
The treatment for arterial ulcers primarily focuses on improving blood flow to the affected area, promoting healing, and preventing complications. Here are some common treatment options:
1. Medications
- Pain management: Non-steroidal anti-inflammatory drugs (NSAIDs) or stronger pain relievers may be prescribed to manage pain.
- Blood thinners: If a blood clot is present, anticoagulants may be used to help improve circulation.
- Antibiotics: If the ulcer becomes infected, antibiotics are necessary to prevent further complications.
2. Wound Care
Proper wound care is critical for healing arterial ulcers. The wound should be kept clean and dressed to prevent infection. Dressings that promote moisture and oxygen flow to the ulcer, such as hydrocolloid or foam dressings, may be recommended.
3. Surgical Intervention
In some cases, surgery may be necessary to address the underlying issue causing the arterial ulcer. Procedures may include:
- Angioplasty: This procedure opens up blocked or narrowed arteries using a balloon or stent.
- Bypass surgery: In cases where an artery is severely blocked, a bypass surgery may be performed to reroute blood flow.
4. Lifestyle Changes
- Smoking cessation: Smoking worsens circulation problems, so quitting can help improve overall blood flow.
- Exercise: Regular physical activity helps improve circulation and may prevent further ulcer formation.
Prevention of Arterial Ulcers
Prevention is key to managing arterial ulcers, especially for individuals who are at high risk due to conditions like diabetes or PAD. Here are some preventive measures:
- Monitor blood sugar levels for individuals with diabetes.
- Manage cholesterol and blood pressure levels to reduce the risk of arterial disease.
- Wear compression stockings as directed by a healthcare professional to help with circulation.
- Inspect your legs and feet daily for signs of ulcers, especially if you have diabetes or peripheral artery disease.
Conclusion
Arterial ulcers are a serious condition that requires immediate attention. By understanding the differences between arterial and venous leg ulcers, as well as recognizing the symptoms and treatments, patients can make informed decisions about their healthcare. If you or someone you know is experiencing symptoms of an arterial ulcer, it’s important to consult with a specialist, such as Dr. Rajendra Bansal, who can provide the necessary guidance and treatment options to prevent further complications and promote healing.